Beyond Words - Why Healing Trauma Needs More Than Talking
Traditional talk therapy needs words. But healing needs more than just words.
When training as a therapist, I was encouraged to let my client ‘take the lead’ in talking. It was my job to listen and pay attention to their feelings and experiences.
I soon discovered that this approach is all wrong when working with trauma.
Keep reading to discover more about why traditional talk therapy can be counterproductive in healing trauma, why this is, and why a different approach is needed.
Talking about trauma
If therapists focus on just listening or encourage a client to describe a traumatic experience before they feel ready, it can make the issue worse.
After surviving sexual assault, Emily – a fictional client – struggled with panic attacks, nightmares, and a constant sense of danger. She also experienced a deep sense of guilt and shame about what happened. Encouraged by friends, she started talk therapy. The therapist encouraged her to ‘process’ her experience by sharing the details of what happened. But Emily found herself shutting down, feeling agitated, panicky and unable to think clearly. Instead of relief, each session made her feel worse. She was either flooded with emotions or disconnected, the nightmares and flashbacks continued. Emily felt like she was failing at therapy. Eventually, she stopped going.
Emily was asked to describe her traumatic experience. Most therapists are trained to ‘listen’ and trauma-informed therapy doesn't feature in many counselling training courses. It also used to be thought that trauma could be healed by just talking about it.
To understand more about why talk therapy didn’t work for Emily, we need to know more about how the brain responds to traumatic events.
Your brain’s response to trauma
Talking requires thinking. And if you’ve experienced trauma, being asked to talk about it can feel so frightening and threatening that your brain can literally ‘shut down’.
The reason is that research of brain scans shows that trauma impacts the prefrontal cortex, a region responsible for many cognitive functions. It shuts down as a survival mechanism, because in the face of threat there’s no time for thinking! It’s time to act.
Perceived threats trigger the amygdala – the brain’s fear centre – to switch off the pre-frontal cortex and ready the body for action. The amygdala becomes more active after trauma, amplifying the triggering of stress responses to stimuli perceived as threats.
Because these are instinctive, physical responses that don’t require rational thought, it’s difficult to approach trauma healing from a place of ‘thinking’.
So, in a nutshell, being asked to talk about trauma is a reminder of it, which can mimic the traumatic experience and exacerbate the symptoms.
Beyond talking
As an alternative to traditional talk therapy, I work in ways that prioritise safety and stabilisation by working with clients to regulate nervous system responses that are triggered by reminders of trauma. This is a necessary precursor to processing the traumatic experience later in therapy.
So, in early trauma therapy the emphasis would be on addressing traumatic symptoms such flashbacks, nightmares or panic attacks as these can make you feel unstable and frightened.
Controlling emotions
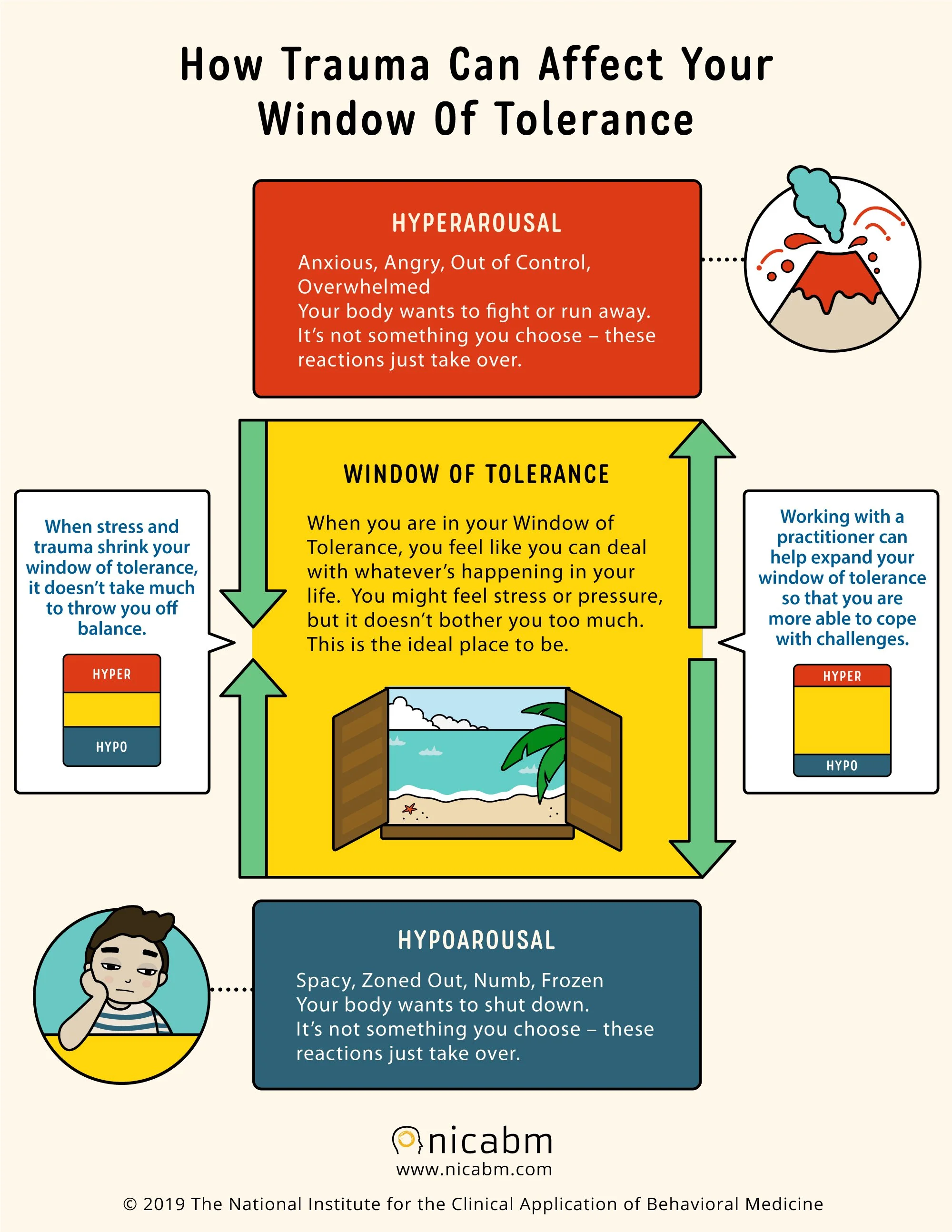
One aim is to help clients widen the Window of Tolerance (WoT). This is your emotional bandwidth – a state in which you can tolerate emotions and still engage in everyday life. As you can see from the diagram, when in this window your nervous system is balanced and well regulated, and the pre-frontal cortex is online.
Trauma dysregulates the nervous system because it alters the perception of danger. This narrows the Window of Tolerance making hyper-arousal (anxiety, panic, anger) or hypo-arousal (numbness, dissociation, withdrawal) more likely.
Helping clients to recognise when they feel too much (hyper-arousal) or too little (hypo-arousal) – which happens outside the WoT – is a critical aspect of stabilisation. I ask my clients to tell me how they might get a better sense of this by noticing physical signs like rapid breathing, muscle tension, or lack of eye contact.
How can you know when you are moving outside this window i.e. what are the early signs for you?
Normalising your responses to trauma
Another key aspect of my trauma therapy practice is helping clients to learn that the symptoms of trauma make perfect sense as a response to a traumatic experience – i.e. they are normal.
E.g. flashbacks indicate that a memory of trauma has been triggered by something in the present. And hypervigilance – another common symptom of PTSD – happens because you’ve learned that you may need to protect yourself from further traumatic experiences. You can learn more here.
Processing trauma
Once my clients feel ready – which differs for every client – a key part of trauma therapy involves helping them to process their experiences.
While the early stages of trauma therapy involve preparation and addressing everyday challenges, this is often when the real healing lies because it involves coming to terms with the underlying trauma which affects your day-to-day life in many ways.
While processing can involve some talking, which can be important for sharing your story, the primary method I use in my practice is Eye Movement Desensitisation and Reprocessing or EMDR. At the heart of EMDR therapy is the theory that present issues (e.g. anxiety or intrusive thoughts) are rooted in unprocessed experiences. So, processing them leads to healing.
And EMDR doesn’t ask you to share all of the details.
Why we need EMDR therapy
Traditional talking therapy has been around since the time of Freud in the early 20th century. But today we know much more about how the brain responds to disturbing, or traumatic experiences and as somebody who trained as a traditional psychotherapist, I can say that training in talk therapy hasn’t kept pace with this knowledge.
Having become a qualified trauma therapist and EMDR therapist, I’ve learned that EMDR therapy is grounded in a biological understanding of trauma. So, it has a model of healing already built into it.
Final thoughts…
If you’ve ever felt like talk therapy just didn’t help, or even made things worse, you’re not failing at therapy. The truth is that trauma affects the brain and body in ways that make traditional talk therapy less effective, and sometimes even retraumatising.
Instead, effective trauma therapy prioritises nervous system regulation and emotional stabilisation. Your reactions are not weaknesses, but natural survival responses. By working with your nervous system, expanding your Window of Tolerance, and helping you to feel safe again, therapy becomes a process of empowerment rather than reliving the past.
When the time is right, EMDR can help you process trauma in a way that feels manageable. There is a path forward. One that goes beyond words and leads to genuine healing.
If talk therapy hasn’t worked for you – it’s because trauma healing needs more than just talking. If you’re ready to explore an approach that prioritises safety, regulation, and true healing, I invite you to take the next step. Please get in touch with me.